Chronic pain is a condition that affects millions worldwide, and finding effective treatments can feel like navigating a maze. Recent innovations in spinal cord stimulators (SCS) and non-invasive neuromodulation devices are giving patients more options than ever, offering new ways to manage chronic pain with fewer side effects. In this article, we explore how these advancements are shaping the future of pain relief.
Neuromodulation is a medical technology that alters nerve activity through electrical stimulation. By targeting specific nerve pathways, these devices can disrupt pain signals before they reach the brain. This means less reliance on medications like opioids and more targeted pain relief.
For patients with chronic pain that doesn’t respond well to medication or surgery, neuromodulation offers an alternative. From treating back pain to managing complex regional pain syndrome, these devices can provide relief where other treatments have failed.
Historically, pain management has relied heavily on medications, physical therapy, or invasive procedures. While effective for some, many patients experience adverse side effects, addiction issues, or limited relief. In recent decades, neuromodulation has grown in popularity as a minimally invasive option for treating chronic pain. It provides long-term relief without the systemic side effects that come with medications, offering patients a more sustainable approach to pain management.
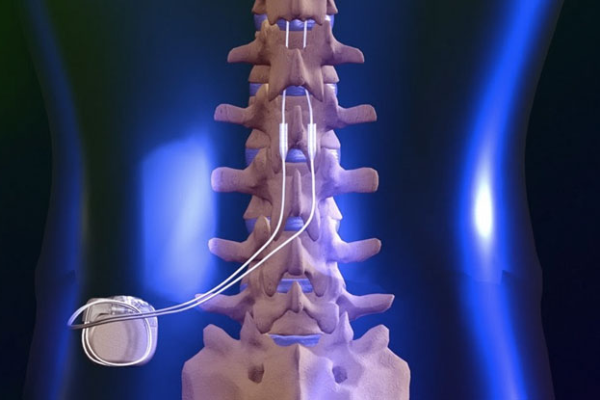
Spinal cord stimulation (SCS) is a type of neuromodulation that involves implanting a small device near the spinal cord. This device sends mild electrical impulses to the nerves, interrupting pain signals before they reach the brain.
The device consists of a small pulse generator and thin wires, called leads, or electrodes which are surgically implanted in the epidural space along the spine. The patient controls the electrical pulses via a remote control, adjusting the intensity to suit their pain levels.
SCS is typically recommended for patients with chronic pain that doesn’t respond to conservative treatments, such as back pain continuing despite previous (often multiple) spinal surgeries, neuropathic pain, and complex regional pain syndrome. Recent advances in SCS technology have enhanced device performance and patient outcomes. Modern stimulators are smaller, more efficient, and capable of delivering a wider range of stimulation patterns.
Newer devices offer high-frequency stimulation, and advanced stimulation protocols, which avoids the related sensation that some patients find uncomfortable with traditional SCS. Burst stimulation is another innovation, mimicking natural nerve firing patterns to provide more effective pain relief.
Personalization is key. With advancements in programming, SCS devices can now be tailored to each patient’s specific pain patterns, allowing for more precise pain relief that adapts to their lifestyle and activity levels.
For those hesitant about invasive procedures, non-invasive neuromodulation devices are an appealing alternative. These devices use electrical or magnetic stimulation applied externally, with no need for surgery. TENS is a well-known non-invasive option. It involves placing small electrodes on the skin to deliver low-voltage electrical currents, which can help relieve pain from conditions like arthritis or muscle injuries.
One of the biggest advantages of neuromodulation is the reduction in side effects compared to traditional treatments like opioids. By directly targeting the nerves, neuromodulation bypasses many of the issues associated with systemic medications. Neuromodulation can be tailored to each patient’s needs. Whether through adjusting stimulation patterns or customizing device settings, patients get a more individualized treatment plan that adapts to their condition.
OVER THE HORIZON
As technology continues to evolve, we can expect more refined and effective neuromodulation devices. Miniaturization, longer battery life, and wireless capabilities are just a few trends on the horizon.
Emerging technology includes:
rTMS uses magnetic fields to stimulate nerve cells in the brain. It’s primarily used to treat depression, but recent studies suggest it could be effective in managing chronic pain as well.
Artificial intelligence is set to play a major role in the future of pain management. AI algorithms could be used to predict pain patterns, optimize device programming, and even automate adjustments for real-time relief.
Neuromodulation represents a promising frontier in chronic pain treatment. With advancements in spinal cord stimulators and non-invasive neuromodulation devices, patients have more options than ever for managing their pain. These technologies not only offer more precise and personalized treatment but also reduce the risks associated with traditional pain management methods. As innovations continue, the future looks bright for those living with chronic pain.
The content provided here reflects the author’s personal thoughts and opinions and is not intended to be taken as medical advice. All readers are encouraged to seek their own individual advice from qualified healthcare professionals for any medical issues or concerns. The information shared should not replace professional consultation or treatment.